Carotid Artery Blockage
What are the causes of carotid artery blockage?
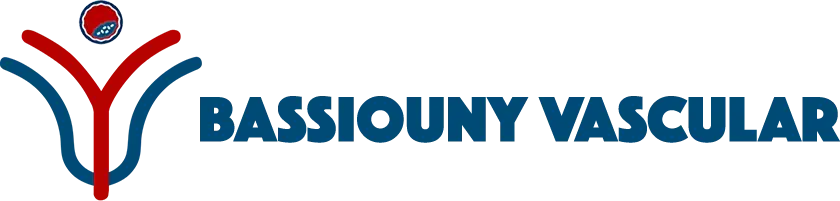
The brain and eye, two of the most vital organs in the human body receive their blood supply via 4 major arteries (left and right carotid and vertebral arteries) that travel thought the neck. (Fig. 1)
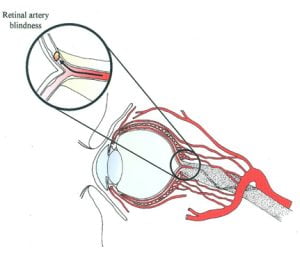
Blockage of such vital arteries could prevent blood flow to the brain and eye which can lead to stroke, most commonly, or blindness.
The most common cause of carotid artery blockage is atherosclerosis. Other less frequent conditions that may block the carotid arteries include carotid aneurysm, autoimmune arteritides, and dissections. Such conditions may also pose a risk to the brain or eye.
How does a carotid artery blockage produce stroke or visual field deficits?
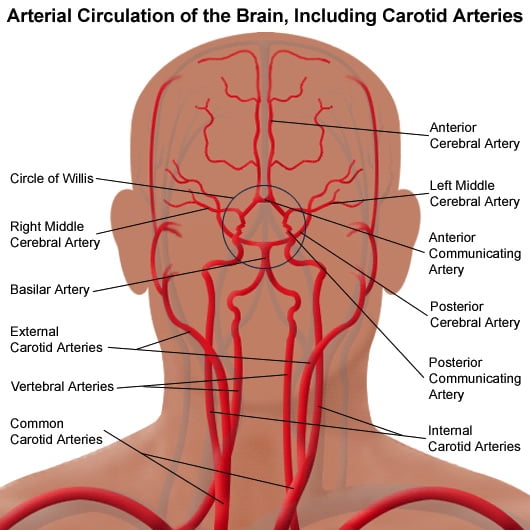
In most cases the plaque producing the blockage may breakdown releasing particulate matter or clots that travel with the blood stream to block smaller arteries supplying the brain or retina (Fig 2,3 respectively). The risk of stroke increases as more than one vessel is blocked. The most common location of blockage is the carotid artery in the neck.
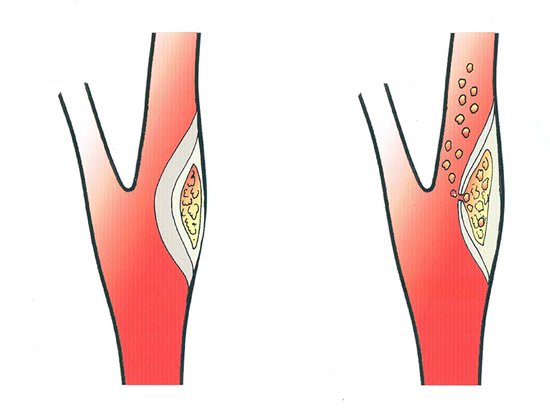
About 20-30% of all strokes are attributed to significant (> 50%) blockage of the carotid arteries in the neck.
It is important to know that carotid plaques have varying structure. Some plaques are soft, inflamed and prone to breakdown and clot formation while others are hard, calcified and have a stable structure. Thus, for a certain degree of narrowing one plaque may be unstable and prone to rupture or has ruptured releasing clots to the brain that produce a stroke (Fig 4, right) while another plaque is stable and likely to remain asymptomatic for the life of the patient (Fig 4, left))
How is carotid disease detected and who should be screened?
Any patient who has suffered upper or lower extremity weakness or diminished sensation i.e., numbness, speech difficulty, visual field deficits symptoms whether permanent (stroke) or reversible (TIA) should undergo carotid duplex ultrasound (US) to determine if there is significant blockage. Duplex US is a non-invasive study that is performed without giving any dye or exposing the patient to irradiation.
Additionally, a CT angiogram or MRI of the brain is essential to confirm the location, severity and structure of the blockage determine which region and extent of brain is involved.
A cardiac cause should also be ruled out clots can originate from the heart and travel to the brain due to arrhythmias or after a heart attack.
Carotid blockage may exist as previously mentioned without symptoms. So, who should be screened by duplex US; the following:
a) Patients with known coronary artery, peripheral artery disease, aortic aneurysms
b) Hearing a carotid bruit on physical exam.
c) Age 60 and above with longstanding atherosclerosis risk factors (smoking, hypertension, hyperlipidemia, diabetes, or thrombophilic disorders.
Management of carotid artery blockage?
Management depends on
- Symptoms.
- Degree of carotid artery narrowing and progression over time
- Type of carotid plaque
- Additional blockage of one or several arteries supplying the brain
- Overall patient risk profile.
Patients who are ASYMPTOMATIC, who are found 50% blockage of the neck internal carotid artery by ultrasound or CT should be treated conservatively by BP and diabetes control, smoking cessation, antiplatelet and statin therapy. Such patients should be followed closely every 3-6 months for symptoms and for evaluation of the blockage by duplex ultrasound.
In select ASYMPTOMATIC patients’ intervention by stenting or surgery may be necessary. These include patients with more than 70% who are low risk for intervention, if their rapid progression of the blockage by serial ultrasound or if there is evidence of a soft plaque or clot which may produce a future stroke.
In SYMPTOMATIC patients with more than 50% blockage of the cervical internal carotid artery who have suffered a reversible or a fixed non disabling stroke or related eye symptoms MUST consider correction of the blockage by surgery or stenting.
Stenting or surgery; which is better?
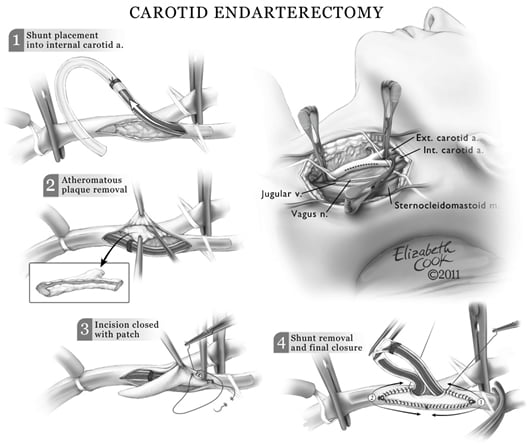
Surgery for removal of the carotid blockage remains the gold standard and is generally associated with a lower risk of stroke during the procedure than stenting. Current practice guidelines (Updated Society for Vascular Surgery guidelines for management of extracranial carotid disease – PDF) indicate patients who are high risk for surgery should undergo stenting.
High risk patients for surgery include those with compromised cardiac function, previous surgery or irradiation to the neck, a carotid blockage that is difficult to reach by surgical means. In such instances stenting is preferred. Stenting is contraindicated if their significant renal insufficiency or atherosclerosis of the arch and difficult anatomy
Operator experience with both procedures is critical in reducing complications with either procedure. The major risk during either procedure is stroke which occurs if a fragment of the plaque or clot breaks of and travels to the brain during surgery or stenting. In high volume centers such as Dar Al Fouad Hospital Egypt, the risk of stroke with surgery is 2% or less and with stenting 4% or less.
In either case the best outcomes are achieved by proper procedure selection for each individual patient. It is therefore critical for the patient to seek care by a vascular specialist who is competent in both procedures and unbiased for either technique.
Surgery is commonly performed under general anesthesia and in my practice a temporary shunt is utilized to maintain blood flow to the brain while the carotid artery blockage is being removed ( Fig 5) The procedure can also be performed under regional anesthesia, however this can lead to significant patient anxiety and discomfort.
Stenting is performed under local anesthesia and a protective filter is placed beyond the blockage to capture any particles released from the plaque during deployment of the stent.
Patient preparation – for surgery
Patients are admitted the day prior to the procedure. It is advised that platelet agents like Plavix are stopped one week prior if possible.
Cardiac risk assessment and evaluation by the anesthesia team is undertaken prior to the operation. Following the procedure, the patient is routinely monitored in the ICU for 6 hours for blood pressure surveillance and control.
A surgical drain during surgery and is removed the following day.
The hospital stay lasts for 1-2 days after which the patient returns for outpatient follow up in one week.
At one month a repeat duplex Ultrasound is performed to check the surgery site and to make sure that the artery is open with no residual blockage.
Patient preparation – for stenting
Patients admitted the day prior.
Routine blood tests are performed to assess kidney function as the procedure requires injecting iodinated dye.
A loading dose of 300mg Plavix is given if the patient has not received the drug prior.
Patients are discharged the after 24-hour observation and return for a follow up scheme as surgery.