Aortic Aneurysms
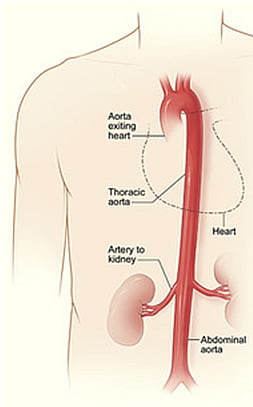
What is an Aorta?
The aorta is the largest artery in the body. It originates from the left side of the heart and carries blood rich in oxygen. The aorta has many branches which carry oxygenated blood to vital organs such as the brain, liver, kidneys, intestines, and extremities. The aorta starts above the aortic valve and courses upwards towards the head then curves and courses downwards thru the chest and abdomen.
What is an Aortic Aneurysm (AA)?
Aortic aneurysms (AA) result from weakening of the aortic wall. The weakened wall stretches under blood pressure and balloons outwards. The larger the aneurysm or balloon the higher the risk of rupture. Rupture causes massive internal bleeding and death in the majority of patients.in the human body aneurysms occur most frequently in the aorta.
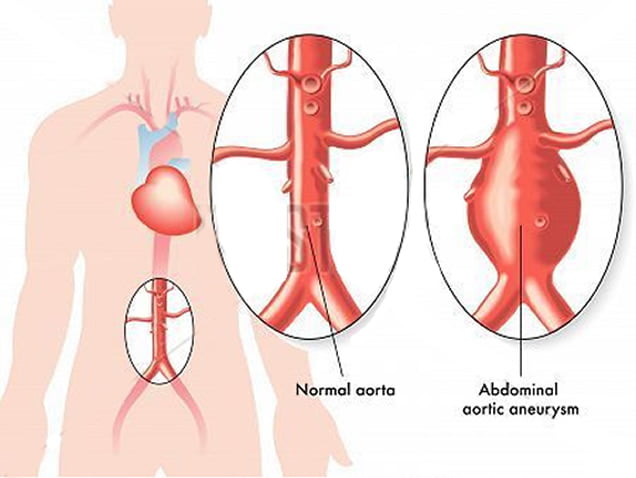
At what level does the Aortic Aneurysm (AA) develop?
The most common location for an aortic aneurysm is the abdominal segment below the kidney arteries. Less frequently AA’s involve the thoracic segment. An AA may also involve both thoracic and abdominal segments at the same time.What are the symptoms of an Aortic Aneurysm (AA)?
AA produce no symptoms whatsoever until rupture occurs or in some instances rapid growth in size, a sign that the AA is about to rupture. AA’s have been coined” the silent killer” because an AA may rupture before one knows that the condition even exists.
Symptoms of rupture or rapid growth vary according to where the AA is located:
Abdominal Aortic Aneurysm (AAA): pain in the abdomen shooting to the back and chest.
Thoracic Aortic Aneurysm (TAAA): pain the chest shooting to the upper back which may extend to the jaw, sternum, and abdomen.
If most AA have no symptoms how are they found ?
In most cases a silent AA is found by coincidence when a patient undergoes radiologic evaluation by Ultrasound or CT for another disease.What causes weakening of the Aortic wall to form an Aneurysm? Who is at risk and how can AA be screened
In most instances (at least 70% of cases) AA develops when the wall is weakened by deposition of fat, inflammatory cells, calcium, and reactive division of the muscle layer cells of the aortic wall. This complex process is known as atherosclerosis or hardening of the arteries. Many enzymes which dissolve the extracellular matrix which hold the aortic wall together are generated as atherosclerosis progresses.
Smoking, diabetes, hypertension, increased cholesterol, are the commonest risk factors for atherosclerosis. AA are at least 5 times more common Males are 5 times more commonly affected than females.
Less frequently the cause is genetic, AA can run in families and a history of an AA should trigger aortic US screening of siblings.
How are AA treated once discovered?
In small AA (5cms or less), close observation with US evaluation is recommended every 6 months. If the aneurysm grows by 0.5 to 1 cm, then CT angiography is recommended.
In addition risk factors such as smoking, diabetes, hypertension, hypercholesterolemia should be strictly managed and controlled. Smoking cessation is paramount.
Intervention to repair AA is indicated in:
a) Large AA (> 5ms in the abdomen or > 6cms in the chest)
b) Small AA with abdominal / back pain or rapid growth.
Treatment plans include:
a) Open repair
b) Endovascular aneurysm repair, EVAR
Both procedures carry better than 97% success in centers of excellence.
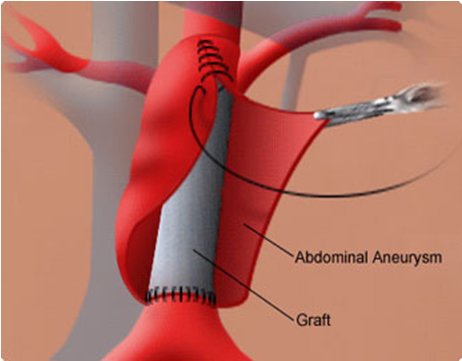
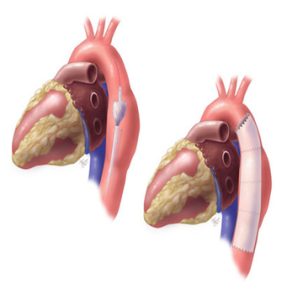
Treatment I. Open repair
The FIRST conventional technique involves replacing the ballooned or dilated segment with a synthetic tube. This requires an open surgical incision in the abdomen under general anesthesia.
Estimated length of stay in uncomplicated repairs is 5-7 days. It is a major operation and full recuperation takes 2-4 weeks after discharge from the hospital.
Major advantages are long term durability and survival. The procedure is reserved for patients with good cardiopulmonary function.
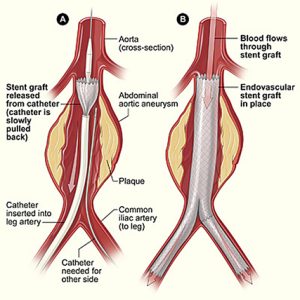
Treatment II. Endovascular aneurysm repair or EVAR
The SECOND technique (endovascular aneurysm repair or EVAR) involves implantation of a covered stent from within the aneurysm sac to exclude blood flow and pressure from the AA thereby reducing tension on the weakened wall and greatly minimizing the risk of rupture.
This technique is minimally invasive and is now used in 70% or more of patients with abdominal, thoracic and thoraco-abdominal aneurysms. The stents are inserted into the aneurysm sac by special catheters that are guided with X ray imaging. Minimal incisions are sometimes needed in the upper thigh region to introduce the stent graft.
Endovascular repair requires precise size planning to ensure complete exclusion of the AA and associated iliac aneurysms if present.
Endovascular stent graft technology has seen tremendous technologic advances in the last decade. Currently stent grafts can be tailored treat AA involving aortic segments with vital branches to the liver, gut and kidneys branches.
The stent graft procedure can be performed under local, spinal or general anesthesia.
Patients who undergo endovascular repair need serial long term follow up with CT or Ultrasound to detect any serious leaks around the stent back into AA as this occurs in 5% of patients
What to expect from open repair?
Admission 2 days prior to the procedure for preparation:
- Blood picture, liver functions, kidney functions and coagulation
- ECG
- Echocardiograph
- Chest X-ray
Assessment of operative risk by cardiology, anesthesia, and internal medicine.
Tight control of blood pressure and blood sugar before procedure.
Availability of adequate type and cross-matched blood.
Every patient is routinely observed from 24-48 hours after the procedure in the intensive care unit then transferred to a regular floor.
Provide necessary pain control.
Hospital stay ranges 5-7 days.
After discharge 2-4 weeks of recuperation is anticipated at home before resuming full activity.
Follow up outpatient clinic visits at 1 week, 1 month, 6 months then every year.
What to expect from endovascular repair?
Admission 2 days prior to the procedure for preparation:
- Blood picture, liver functions, kidney functions and coagulation
- ECG
- Echocardiograph
- Chest X-ray
Evaluation by anesthesia and nephrology prior to procedure.
Choice of anesthesia discussed with patient) local, general or spinal).
The endovascular repair is performed by introducing the stent graft through the upper thigh artery by 2cm incisions.
Expected stay in the hospital is 2 days. Return to work and regular activity in one week.
At one month and yearly thereafter the stent graft is evaluated by US or CT to assess position and the presence of any leaks which may cause the AA to regrow.